Blog
Sjogren’s Disease: Autoimmune dry eye Part 4
When we consider the regulation of tearing and salivation (mouth moisture, AKA spit production), these functions are under the direction of the so-called autonomic nervous system. This is the collection of nerves connecting our brain with the visceral organs (basic breathing, heart beating, digestion, etc.) as opposed to the nerves connecting the brain with our skin and muscles (the somatic nervous system). Autonomic is equivalent to “automatic” and allows our body to function without conscious thought.
Sjogren’s disease can damage and “reprogram” this autonomic nerve control and according to a neurologist, Dr. Goodman, specializing in this branch of the nervous system, it can account for or cause nearly any neurological syndrome. He postulated an interesting concept – wondering if the autonomic nervous system might be able to “prime” the immune system (where conventional thought would be the reverse (that the immune system might damage or reprogram the nervous system). This would allow for what he terms “maladaptive remodeling,” where the nervous system “learns” to behave badly.
Additional thought from the GI doctors, is that the gut “microbiome” (the germs that populate our intestines and are important to our digestion, nutrition, and general well-being) may contribute to the autoimmune response. This makes sense, as the body’s reaction to germs is an innate immune response and will begin interacting at the first contact with germs – including – and perhaps especially – to those in our gut. The defenses we mount include small chemicals (cytokines) that can be released into the circulation and find their way throughout the body – including the eyes, mouth and nervous system. At the level of the gut, we find Sjogren’s causing a dry mouth, GERD – an improper movement along the GI tract resulting in reflux from the stomach and up the esophagus. The stomach can become inflamed (gastritis), and often gets “run over” by a common germ, H. Pylori, which has been associated with stomach inflammation as well as Rosacea and a variety of other ailments. Further inflammation can target the gallbladder, pancreas, liver, small and large intestines – causing havoc along the entire digestive system.
Dr. Robert Fox, a rheumatologist specializing in Sjogren’s, points out that headache is a common manifestation of this disease. Interestingly, the Trigeminal nerve – the main sensory nerve of the face, which also supplies pain feelings from the eyes – under stress from Sjogren’s, releases small protein complexes called Calcitonin Related Group Peptides (or CGRPs) that enter the brain (at the thalamus) and can dilate blood vessels which can trigger migraines and can start a cascade of pain signals including pain in the eyes and photophobia (eye pain from light). At the same time as these amplified pain signals come along, there is a second small protein (Pituitary Adenylate Cyclase-Associated Peptides, or PACAPs) that lowers the threshold to feel pain related to light, sound and muscle activity. It can also be associated with so-called “brain fog” common to those suffering from Post-Traumatic Brain Syndrome, or Post-Traumatic Stress Disorder (PTSD). This compound is also found in the tear and saliva gland regions of the Trigeminal Nerve and may release into the same (thalamus) portion of the brain responsible for sensing pain – and decrease pain thresholds (so a little pain can go a long way towards hurting).
Unfortunately, there appear to be many routes to fatigue and brain fog – including autoantibodies and depression – so there does not appear to be a “silver bullet” for fixing these problems. Dr. Kate Hackett is a PhD Occupational Therapist involved in dealing with Pain, Fatigue and Sleep. She points out that sleep apnea is more common in the Sjogren’s group – which is of interest to eye doctors, as you recall my post about the “Floppy Lids” that are commonly also related to sleep apnea – so we are more apt to refer patients for sleep studies from a common eye exam. Interestingly, the common recommendation eye doctors make to dry eye patients – about using a humidifier – appears to help patients with Sjogren’s get better sleep. She points out how important it is for patients dealing with chronic pain to get adequate rest and adequate sleep – so finding helpful tools like a humidifier can really help. Also helpful is gentle exercise and taking frequent breaks (what she calls “activity management”). Others also point to the benefits of meditation, yoga, and exercise as possible means to help “reprogram” the runaway autonomic nervous system. There is a subset of Long Haul Covid that can result in an unusual and unwanted sudden increase in heart beating (so called tachycardia) when transitioning between lying down to sitting up (called POTS – a good link here: https://www.hopkinsmedicine.org/health/conditions-and-diseases/postural-orthostatic-tachycardia-syndrome-pots ). This has also been found in some Sjogren’s patients and fortunately the same reprograming from meditation, yoga, and exercise appears beneficial for this syndrome – so all these interventions appear likely to be a mainstay of therapy for so called “autonomic dysregulation,” whether from Sjogren’s (or other diseases like long haul Covid).
______________________________________________________________________________
______________________________________________________________________________
Next week, we will explore: “what does the future look like for Sjogren’s patients?” Fortunately there are new consortiums of research activities that appear to bode well for a good answer.
Sjogren’s Disease: Autoimmune dry eye Part 3
Part 3
Sjogren’s Disease is associated with other autoimmune diseases in 52% of cases – so once I identify a patient with Sjogren’s, I always refer to a rheumatologist to assist with further diagnosis and treatments. A group of these “concurrent” diseases include:
- Rheumatoid Arthritis (attacks joints and can cause eye problems like “iritis”)
- Scleroderma (a skin disease resulting in thickened, inflamed skin)
- Celiac disease (true gluten allergy, where G.I. diseases including cancer can be triggered)
- Autoimmune Hepatitis (liver disease)
- Neuromyelitis Optica (mimics Multiple Sclerosis, but treatment is different)
- Autoimmune Thyroid diseases
- Primary Biliary Cirrhosis (another liver/GI disease)
- Systemic Lupus Erythematosus (SLE) – a complicated autoimmune disorder that can cause many diseases involving every major body system.
Some of the manifestations directly related to Sjogren’s include:
- Renal Tubular Acidosis (a kidney disease)
- Interstitial Nephritis (another kidney disease)
- Cystic Lung disease
- Cryoglobulinemic Vasculitis (where inflammation in the blood vessels can cause a gamut of body-wide illnesses).
A bit more scary, is the increased risk of Non-Hodgkin’s Lymphoma, a rare cancer of the body’s lymphocytes (part of our natural defense system). The Arthritis Foundation has a good page on this here: https://www.arthritis.org/health-wellness/about-arthritis/related-conditions/other-diseases/non-hodgkins-lymphoma-with-sjogrens-syndrome
From that source comes this:
“Not everyone with Sjögren’s has the same risk. Symptoms and factors that raise the likelihood of developing NHL include:
Enlarged salivary glands, especially if they stay swollen for months or years
Persistently swollen lymph nodes (glands) in the neck, armpit or groin
Pinpoint or button-sized areas of bleeding in the skin (usually on the lower legs) called petechiae or purpura
Nerve damage known as peripheral neuropathy
Poor blood flow to the fingers, toes, ears or knees, called Raynaud’s phenomenon
Abnormal proteins called cryoglobulins and/or gamma globulins in the blood
The number of factors you have is key in determining your risk. In people with fewer than two of these factors, the risk for NHL is less than 4%. In those with three to six of these factors, it’s nearly 40%.”
This is another reason I like to refer to a rheumatologist, as they are keyed into these (potentially many,) Sjogren’s-related issues and are in a better position to diagnose and properly refer or treat them, if they are found present.
A clip from an American College of Rheumatology meeting abstract has a good description of how rheumatologists (and other medical professionals dealing with Sjogren’s Disease) will look at quantifying signs and symptoms of the disease. The abstract I’m referring to can be found here:
When investigating how much a disease is affecting an individual, it is helpful to have a systematic way of quantifying disease activity – in part to know if that patient is progressing in a way that is better or worse, but also to help validate studies to know if a particular treatment is truly helping populations of patient with the disease. One of the greatest challenges of such studies about Sjogren’s patients, is that they are a diverse group – some of whom have multiple (other) autoimmune diseases, that there are many ways the “same disease” can affect people - and all of whom can have variable degrees of the disease (from a little to a lot) that can vary over time.
We can stratify Sjogren’s to help determine who is best eligible for disease-modifying therapies – as most therapies will target specific portions of Sjogren’s signs and symptoms – and any of them can also have significant side-effects, so patients with less illness will usually want less potentially toxic treatments. The primary disease symptoms are classified as:
- Dryness
- Fatigue
- Pain
And by a Low vs High Symptom “burden” – i.e.:
- Dry with low pain
- Dry with high pain
Disease activity can be categorized:
- Dryness (sicca) alone – without body-wide disease activity or enlargement of the saliva or tearing glands (18%)
- Predominantly dry, but with mild to moderate general body-wide disease activity (especially joint pain, blood disorders and/or gland enlargement = 74%)
- High body-wide disease activity with or without dryness (8%)
On top of this, can be multiple forms of disease affecting peripheral nerves. This is because Sjogren’s can also primarily attack these smaller nerves and affect our sense of balance, our ability to sense or feel things – or can result in a normal ability to “sense” even while depleting the tiny nerve fibers in skin and in the surface of the eye (leading to surface problems and can wreak havoc on those already suffering with dry eyes).
Next week, I’ll focus on more specific issues associated commonly with Sjogren’s and some of the advances in treatments that are underway…
Sjogren’s Disease: Autoimmune dry eye Part 2
Sjogren’s Disease: Part 2 – how it can affect us… Let me count the ways!
In a 2021 United States of America survey by the Sjogren’s Foundation, where they got 3,622 Sjogren’s afflicted patients from this country responding, the age groups who reported varied from 18-94 years of age. Over half believed they had symptoms of their Sjogren’s disease before the age of 35 years, with 16% having symptoms before the age of 18 – so this disease can start early in life! Over 60% had a family history of autoimmune diseases, so there appears to be a genetic predisposition (though clearly there are many cases where there doesn’t appear to be that obvious of a genetic link).
Importantly, while eye dryness was the number one issue for most, over 80% had at least one diagnosed nervous system-related health condition, which could include:
Anxiety or depression (50%)
Brain Fog (47%)
Neuropathy (45%)
Migraine (32%)
Fatigue (25%)
The Sjogren’s Foundation reported 20 clinical treatment trials underway, with 3 of them already in phase 3 testing (so looking near to being approved by the FDA for broader treatment of Sjogren’s Disease). As more treatment protocols become available, it will become increasingly important to accurately diagnose the disease, so it can be staged and properly treated. Treatment will commonly require a competent team approach, usually involving the dry eye specialist for detection and eye treatment, an oral surgeon coupled with a good oral pathologist to help with detection and treatments that may involve a diagnostic biopsy of the mouth’s saliva glands and perhaps opening the saliva ducts inside the mouth, dentists to take care of the frequent cavities and dental decay acquired from a dry mouth, and rheumatologists to aid in diagnosis, staging, and treatment plans related to Sjogren’s and to the many, often associated autoimmune diseases that can run in concert with it. Gastroenterologists, neurologists, pulmonologists (lung), nephrologists (kidney) and sometimes, endocrinologists (especially thyroid) and oncologists can also be needed - depending on the range and severity of the disease.
Diagnosis can be difficult, as blood tests are not always reliable and may miss it (though a positive major antibody test – the so called “Ro” - is considered diagnostic, it is sometimes not found in patients with active disease). Ultrasound of the saliva (the “spit” or “salivary”) glands, including the large parotid glands, may help point to the diagnosis as there are many classical findings (as can also be true for MRI, CT scans, and in the case of lymphoma – a relatively rare cancer that can be more common in some patients with Sjogren’s, then PET scans can be helpful) – but a biopsy of affected saliva glands is still considered the most definite way to diagnose if the blood tests are negative (and requires a good pathologist to “read” the results, as it is easy to over or under diagnose).
So far, unless a patient of mine has very poor “sprinkler system” output (as measured by a very low Schirmer’s test) as well as a history of a very dry mouth (like not being able to swallow a dry saltine-type cracker without water to wash it down), I generally don’t go looking for Sjogren’s with the blood tests - unless there is a poor response to standard initial treatments for their dry eyes. This is because so far, there has not been an acceptable protocol for treatment beyond the eyes – leading me to not go looking for a disease we don’t have a good “fix” for. Adding a lip biopsy to a negative blood test didn’t make sense for the same reason. That may soon be changing as the newer treatments become available, though any patient with severe disease will usually be detected early and referred to the appropriate specialists – as even the imperfect treatments available now are still better than allowing Sjogren’s to “run rampant” in a severely afflicted individual.
Future posts will elaborate on some of the ways Sjogren’s Disease can attack specific body parts apart from the eyes, and I think you’ll soon realize why a team approach is required – since Sjogren’s is so much more than a “Syndrome!” If you or someone you know has Sjogren’s Disease (often referred to as Sjogren’s Syndrome”), then please make sure they check the Sjogren’s Foundation website, since they offer invaluable information and they help keep us all updated on breaking news about this challenging disease.
https://sjogrens.org/living-with-sjogrens?gclid=CjwKCAiAxP2eBhBiEiwA5puhNcqJeHtH9tfIpr769Pb7jjS2_qGTgvtSpk0Q25Fv9dFHjMssbzuykBoC5REQAvD_BwE
Sjogren’s Disease: Autoimmune dry eye Part 1
Sjogren’s Disease - or; When our immune system starts throwing “smart bombs” at our water-producing glands and what that can mean to our eyes (& to our life!).
Until relatively recently, Dry Eye Disease was called Dry Eye Syndrome – probably for several reasons. First, is that we didn’t understand it very well (not to imply we now understand it particularly well – just “better”). Second, saying “disease” sounds more “harsh” or “serious” – while “syndrome” somehow seems less severe or serious - and since we didn’t have a lot of understanding – or ways to treat it - it seemed better to “downplay” it.
This terminology also applies to Sjogren’s Disease, as it was also referred to as “Sjogren’s Syndrome” until relatively recently, perhaps for many of the same reasons. While we now understand it better, we still have a long way to go – and since it can have a huge impact on our being, it is good to know that there are many studies underway to help improve our understanding and give us more tools to treat it.
Early in my posts, I covered the “accidental” damage to our tear glands that commonly occurs when our eyes become dry and irritated, as irritation begets inflammation and inflammation leads to damage to our tear glands. As the glands become damaged, we get more dry and more irritated, which leads to more inflammation and more dryness – the so called “vicious cycle” of dry eye disease. As our immune system spools up, it can act like “gas on the fire” of this vicious cycle.
Sadly in the case of Sjogren’s Disease, our immune system becomes more confused and starts making antibodies that attack the water-producing glands throughout our bodies “on purpose” (versus the more typical “accidental” damage from dry irritation) and can become a hydrant of gas on that fire. This affects our eyes by drying up the water in our tears and since water makes up most of a healthy tear, the tear volume drops and eyes suffer.
But Sjogren’s frequently goes far beyond affecting our eyes, as the white cells (Lymphocytes) from our immune system can also attack our nerves, our organs and especially, our gut. This post serves as a basic introduction - and for future posts, I’ll cover more details about how broadly this can affect us, current aspects of diagnosis and some of the commonly accepted current treatments – but will attempt to touch on some of the newer approaches and possible treatments being investigated.
As these immune cells (Lymphocytes) go after nerves, they will cause an “autoimmune neuropathy” – where nerves can become weaker and lead to numbness or pain (and sometimes, degrees of both). In an earlier post, I noted how corneal nerves are the “maestro” that conducts the “orchestra” of tear production and of the delicate dance of cells that constantly turn over and renew the surface of our eyes. Poor tears can weaken that surface, but when the cells lose their “marching orders” the surface can get very rough and damaged. These eyes may need every trick in our book to survive. Commonly, this includes some degree of anti-inflammatory drops like Cyclosporine, Lifitigrast and topical steroids, biologic support from Autologous Serum Tears and Amnion products and higher levels of attention to ancillary dry eye issues like Meibomian Gland obstruction, Rosacea-related inflammation, blepharitis, allergies and surface issues pertaining to the conjunctiva and eyelids.
I harp on use of preservative free artificial tears (so we don’t punish the tear glands and eye surface with harsh chemicals designed to kill germs that may gain access to the bottles through air or contact of the tip with our eyelids or fingers) – but as a final portion of this post, I will also mention that this opens the door to bad germs gaining access through contamination at the factory level – as appears may be the case from this CDC notice: CDC Urges Discontinued Use of EzriCare Artificial Tears (as they may be the source of some terrible eye infections and possibly one death)! Stay tuned for more…
52.1429 weeks in a year - and this is #52 of my Dry Eye Posts!
Another Happy New Year to you. In reviewing my posts since my start 12/29/21, I noticed this is officially #52 and since Google says there are 52.1429 weeks in an average year, I guess this closes out a full year of my posts. I took the opportunity over the weekend, to read each and every one of these posts and I noticed the common theme - Tears are important as they serve as the “clear blood” serving to support the living surface of our eyes. Blinking is the “heartbeat” that constantly renews and re-distributes that “clear blood” so the surface can stay healthy with those fresh tears.
I also noticed that while I repeat certain information in many of my posts, it comes down to the mainstay of how to help keep tears healthy - so they can support that living surface through the thick and thin of modern life. Such life now lasts longer than prior generations - yet we use our eyes more than any generation before us, thanks to the “digital world” we live in. That kind of stress is bound to show up in a diverse array of ways and can account for the many signs and symptoms relating to unhealthy tears. We dry eye specialists refer to unhealthy tears as “Dysfunctional Tear Syndrome” but call it “Dry Eye DIsease” to our patients, friends and non-dry-eye-specialist colleagues. We refer the outcome of those dysfunctional tears, as “Ocular Surface Disease,” and many of us have devoted much of our careers to better diagnosing and treating it.
Once we accept that tears equal “clear blood,” then it is easier to accept that when tears go bad, the surface of our eyes will “go bad.” Just as “bad blood” can’t support our bodies to stay healthy and will lead to “disease,” this means bad tears will lead to “Dry Eye DIsease” (or whatever we chose to call it).
For any of you in doubt about whether you may have dry eye disease, I refer you back to my first posting, December 29, 2021, https://www.eyethera.com/blog/rn9p8ouyjzjhyfpkvrysxjx28no0q8 where I posted my introduction to dry eye disease and a simple 20 second “test” you can do at home to help you. If any of you find the test pointing in the direction of Dry Eye (or Ocular Surface) DIsease, then if you haven’t done this in a while (as I had not), I will suggest you read through my posts from the start, to present day. I think (and hope you’ll agree) I’ve done a reasonable job at putting it all into some perspective - at what I aim to be the “average patient level.”
Launching my postings into 2023, I will do my best to continue this tradition and help bring newer thoughts, technologies, treatments and perspectives to what I can share. I realize that many of my readers are already my patients, friends, colleagues and family - and I hope to “spread the word” through each of you, to your patients, friends, family and colleagues. Let’s help “stamp out” dry eye and ocular surface disease together!
Do blue blocking glasses help with dry eyes?
As a dry eye specialist, I’m often asked if wearing blue blocking glasses (or adding blue blocking filters to computer screens) can help or prevent dry eye disease. The short answer is possibly, but the better answer follows.
Scientists point to the regulation of our sleep schedule being dependent on a schedule that evolved over eons and was regulated by the sun. Long before we had homes with electricity, we commonly lived in caves or other primitive structures and the day began around the time the sun came up and ended around the time the sun set (or our campfires went out).
The “blue sky” we see in daylight is a strong “wakeup” signal that would prepare us for a day of hunting and gathering that could sustain us and allow our species to survive and thus evolve. At night, a small gland in our brain, called the pineal gland, would begin making melatonin around the time the world went dark and prepared our bodies (and brains) for sleep. As the melatonin seeped into our brain, it functioned as a type of sedative that allowed us to have the sleep-related rest that prepared us for the following day.
Today, our day often begins with an alarm (perhaps set on our smartphones) and with the electric lights coming on – often hours before a full sunrise. Conversely, our day often ends many hours after the sun sets – and during this “artificial daylight” our brains are denied the gradual buildup of that natural sedative (melatonin) that the bright blue sky would stave off so we can hunt and gather. Unless we use programs and filters to block the blue light we see while staring at all the screens that seem to rule our lives, this is a strong source of that “wakeup signal” that makes sleeping difficult.
Sleep is incredibly important to our health in general and to our eye-health in particular. Resting with closed eyelids can help restore the living surface of our eyes, as they are no longer exposed to the drying atmosphere - and the delayed blinking - caused by staring and visually concentrating while awake. Video screens (phones, computers, tablets, and laptops as well as TVs) are a great incentive to staring – and as I pointed out in earlier posts – staring is like giving your eye’s surface a “heart attack” as blinking is the “heartbeat” that churns the “clear-blood-like product we call a tear” over on the surface of your eye to sustain and support it.
The principal benefit of blue-blocking-glasses (or screen covers/filters) appears to be the return of the melatonin-related regulation of our sleep cycle – and the return to better sleep and better health. This is especially useful once the sun sets, so some computers have settings where you can reduce the blue in the screen automatically. Lighting can be dimmed around the house after sunset and aiming for the number of hours of sleep you need can be an easier task.
The limiting of screen time, the 20/20/20 “rule” of taking 20 seconds every 20 minutes to look 20 feet or further away (and doing some strong blinking to promote the function of the lid’s oil glands) is also helpful to maintaining healthy tears and therefore healthy eyes.
So do blue blocking glasses help dry eyes? If you, like most of us, spend “too much time” after dark, staring at screens that have the full spectrum of natural colors (including that bright blue-sky blue), then definitely consider blue blocking strategies and get some sleep!
More on MGs (the tear oil glands)
In dry eye patient chats, I commonly come upon questions like - “My doctor says I’ve lost a lot of my Meibomian Glands. How many MGs do I need to have a good tear?” And: How fast can they disappear?” “How do I get them back?”
Dr. Donald Korb is the Optometrist who invented Lipiflow (the first well-sorted tool to provide a good heated expression for obstructive MGD). He is a great observer and excellent researcher. He is also the one that told me 6 good MGs/lid is sufficient to support an adequate tear (usually measured by the tear break up time and lack of dry spots on the cornea). I don’t believe this has been supported in peer reviewed studies but based on his expertise and my clinical observations, I can say that I believe this to be true. That’s good news for those struggling to keep 6 or more well functioning glands. This doesn’t necessarily speak to the quality of the oil, the constitution of salts and proteins nor the volume of water that is the bulk of a tear. It also is bad news for patients who don’t yet have a handle on the number of glands they still have, as most people have 25-30 glands per lid at birth. If you’re down to your last 6 good glands, life is good until you lose one more gland. So the short answer is that it is best if you can hang onto more than 6 and keep them in good shape.
It would be unusual to lose 50% of the MGs in 6 months (or even a year, since it appears to take years-to-decades for the average dry eye sufferer to see major losses) - but in cases where blinking is severely impaired - like a Bell’s Palsy - or in cases where medications like Accutane have been used, I believe it may be possible to lose as much as 50% in less than a. year. Sadly, the imaging used to detect the glands is far from perfect and the state of MG activity appears to greatly influence how "white" (and therefore detectable) they appear on InfraRed photography (the standard way of imaging them). If you can support them with adequate Omega Oil supplements, warm moist compresses with "lid crunches," blink exercises and good lid hygiene after ensuring adequate purging of obstructions, then I have found it is possible to see many of these ghostly MGs "bounce back."
Regeneration of the glands remains controversial, but it does appear that glands that are not “too far gone” can bounce back if given the chance. In general this means adequate unclogging and then adequate “homework” as I outlined in earlier postings. IPL appears uniquely suited to stimulate them, and Maskin Probing is sometimes required to sufficiently unclog them, but a good heated expression is often needed with or without the probing and IPL treatments. Best to work with a good dry eye specialist and do the homework.
How Safe and Effective are Home-Based Radiofrequency and Light Treatments for Dry Eye Care?
Happy New Year! I thought it would be appropriate to start the new year with a common thread among some dry eye sufferers I’ve advised over the past year. The common question is – since office-based treatments are so expensive and because some similar technologies are now being offered for self-treatment home care – why can’t I just buy a radiofrequency unit and a light-based unit, and do my own treatments? These treatments could perhaps replace some office treatments, or be used as an office treatment “extender,” or optimizer?
When a particular RF unit was singled out, I found an Amazon link to an eerily similar device for $99. There was very poor grammar in their marketing brochure, suggesting a poor understanding of English language. Some foreign countries have substantial road blocks to product liability and if they fry some eyeballs, there isn’t much recourse. A FB post I did to address a question from a dry eye sufferer helped explain my take on these cheap, “fix it at home” technologies:
I can’t speak to specific “Over The Counter” (OTC) products like this one, but generally speaking, the aim of RF (off label, as it has yet to be studied and approved for this use by the FDA), is to heat directly over the eyelid area, to melt and allow adequate expression of the waxy obstructions in the oil glands of the tear system. Because RF can penetrate deeply through the skin and eyelid tissues, I’ve found it extremely useful for this purpose. I also used special thermal imaging cameras to track this temperature and found if you don’t get to the common “melting point” of the waxy plugs obstructing these glands (around 42-43C) then you never really get that adequate expression. That same temperature can also affect the cornea or clear “window” of the eye, as it resides directly under the lids. Doctors using this technique will use special eye shields to protect the cornea and to assist in the expression of the waxy obstructions. The OTC tools I’ve seen do not appear to have a temperature monitoring system (it goes off by time and not the temperature) so it is hard to know if they can unclog the glands. They also doesn’t have anything to protect the cornea if you do get it that hot, so I personally cannot endorse them. As far as getting the aesthetic benefits, the prescription strength RF devices have good scientific studies to back up true clinical results we see but I didn’t see any such studies for the OTC units. Any form of deep heat can temporarily improve the appearance of fine lines and wrinkles by swelling the skin, but the long-term improvement comes from the specific stimulation of the cells that make and repair collagen and elastin. I’d be interested to see peer reviewed, dry eye studies using these home-based, OTC units. I’m working with some RF companies (as are other doctors) to increase acceptance of RF worldwide for dry eye treatments, which requires ongoing studies and training specific for dry eye diseases.
Low Level Light Therapy (LLLT) is a world-wide growing trend, using relatively low levels of light in certain spectrums found to benefit a variety of medical ailments. LLLT encompasses a wide range of light energies and spectra and has many scientific studies to support biological influences that may be beneficial for a wide range of problems (& some units may have been FDA approved for the treatment of those problems - so the manufacturer can claim it is FDA-certified) – but as far as dry eye disease goes, it has no where near the level of study (nor specific FDA approval for that specific indication) as many other treatments, including IPL, which was approved over a year ago, specifically for the treatment of dry eye disease.
There are numerous anecdotal reports and some limited published reports of dry eye benefits, so some companies are selling these units to eye doctors – and while there are an increasing number of those doctors using this technology for the purpose of treating dry eye, I have not been able to find enough peer reviewed, scientific data to support the safety and efficacy of LLT for dry eye-related disease. At least the majority of these office-based “eye” units have been specifically tested for eye safety and have USA-based companies representing them, – so product liability is likely to be well regulated. Units you can buy and use at home can provide over 10,000 lux of light energy – and that amount of light energy is certainly sufficient to cause harm to an eye if not appropriately shielded. Filters can bring that light into a spectrum like an IPL’s when treating dry eye – so while there may be efficacy for some units – the proof of safety and how well they work remains to be sufficiently validated before many of us would recommend it for our patients using office-based care – and even more so for home-based treatments.
As usual, I recommend working with a dry eye specialist who can offer a range of proven dry eye care treatments, who can take some time to answer your questions and provide a well explained treatment plan specific to your dry eye needs.
Here’s to a healthier, happier 2023!
Why do some people produce “pasty meibum?” PART 4
Part 4:
This brings us to the issue of lid hygiene. Germs feast on our oils and Demodex likes to feast on the germs fat on our oils, as well as feasting on those oils, themselves. Rosacea-related - and many other cases of dry eye disease-related - inflammation is commonly stirred up by those germs and particularly by the Demodex mites involved with those germs. Based on what I've read about Demodex and rosacea - and given the near pandemic of rosacea I find in the northeast, I think there is good reason to prescribe anti-Demodex therapy for those who have rosacea and/or MGD. (I've heard statistics that suggest that we may all get infested with Demodex if we live long enough – approximately 30% have it by age 30, 50% by age 50 and 90% by age 90.)
I also find it rare to see rosacea patients who don't have some degree of evaporative dry eye disease. (the form of dry eye that comes from too little, or the wrong kind of oils in our tears). Though many have thin, clear oil (if scant), I find frequent soap-suds-like bubbles in their tear film - presumably from bacteria. Demodex can add inflammatory elements to those “clear oils” - making the oil more like “kerosene,” than like the “extra virgin olive oil” you’d prefer in your “salad dressing.” Because of the good luck I've had with Cliradex, I have been reluctant to abandon its use in select cases - but I also find that the Avenova iLid cleanser can work well, coupled with ZocuWipes – and is less irritating to the sensitive skin of most of these rosacea patients. I routinely package these in my dry eye “kits” that can be additionally custom tailored to meet the needs of each patient I see. Topical Ivermectin has shown good activity against Demodex and there is a pipeline drug, likely coming to market within the year. IPL, along with improving the flow of oils (with the many tools available for this) both help control Demodex, along with lid hygiene. Combined with pure Hypochlorous Acid sprays, this is for most) an effective way to control bacteria and mites from adding to dry eye (and eyelid) misery.
To combat this problem, I think we need to better educate patients. Just as we teach kids to eat a less sugary diet, brush and floss their teeth and go to the dentist regularly to save their teeth, we need to do something similar for encouraging better blinks, diets rich in the essential Omegas, physical activity/exercise and lid hygiene to save their eyes. Procedures that melt and express these waxy oils are necessary in the more advanced stages, but if caught early, I believe we can largely prevent MGD - or at least better control it. I’ve used Dr. Korb's technique of debridement of the lid margin as an adjunctive tool to his Lipiflow technology, though as I’ve noted, I’ve published on modifications of this with some off-label use of radiofrequency for a more customizable expression and often combine it with a BlephEx lid hygiene treatment and Intense Pulsed Light Therapy (see my earlier posts on this). It is ironic that the nation leading in health and technology is poised (in some part due to our computer-dependent workforce and lifestyles) to be a nation of irritated, dry eyes - as we fail to properly care for our eyes even as we over-use them and - thanks to every other aspect of modern medicine - begin to outlive our MGs and their basic but critical tear functions. The “homework” I prescribe (and have endlessly posted on) remains the mainstay of what has - for the majority of my patients - been an effective way to support and promote the Meibomian glands and to prevent the “pasty Meibum” that is so common a cause of obstructive MGD and resulting evaporative dry eye disease.
Why do some people produce “pasty meibum?” PART 3
Part 3:
It is clear that there is a significant difference in the composition of oils from those with MGD and those without - and it appears that bacteria may play a major role in some of these differences: I quote from a scientific paper (and add interpretations) below:
"Using the compiled data, the team semi-quantitatively revealed the variety of FAs and OAHFAs (Fatty Acids or FAs and (O-acyl)-omega-hydroxy fatty acids or OAHFAs = building blocks of tear oils) present in MGD-affected human meibum. Overall, they identified 161 molecular species. Of these, 100 were long-chain FAs containing 12 to 37 carbons, which is a marked increase in comparison with other detection methods. The remaining 61 species were long-chain OAHFAs 34 to 56 carbons. The researchers note that a wider mass range could result in identifications beyond the 37-carbon threshold for FAs but indicate that this study is the first report of large numbers of very-long-chain species in human meibum (tear oil). Given the rare nature of species longer than 35 carbons in blood, skin or cell samples, this finding confirms the unusual lipid composition of meibum (tear oil). Interestingly, the team also detected odd-numbered carbon-chain FAs, which previously have been linked to bacteria. Mori et al. recommend further investigation into a potential link between this finding and possible bacterial infection in the eyelids of MGD patients."
(This is one of the reasons I stress good, regular lid hygiene to my dry eye patients.) From: http://acceleratingscience.com/proteomics/meibum-lipid-composition-in-dry-eye-disease/
Once one thinks about the normal, wide range of complex oils in the healthy, human tear, it is easy to understand how difficult it will be to create a sufficient “tear substitute!”
Now that I look harder at my routine patients, I find MGD to be nearly ubiquitous - and prevalent even in those as young as early teens (& probably earlier - I just no longer see young kids in my practice). I think this begins with poor blinking (a subconsciously "learned" response that is encouraged by use of computer-related activities like smart-phones, tablets, video games, computers and the like - and discouraged by outdoor play, where bright lights, wind and vigorous activities encourage better blinking). Inactivity may also lead to reduced blood flow in the lids that may reduce eyelid temperature. Poor diet (the high levels of processed foods in the America diet are said to have reduced healthy Omega oil intake by over 95% compared to 100 years ago, when such processed foods hardly existed) needs to be reversed - with a better focus on good eating habits and proper supplements (I like the MaxiTear Dry Eye Formula, which comes closest to Hydroeye as an all-in-one, based on the work of Drs. John Sheppard and Stephen Pflugfelter, but includes a bit more fish oil, some Curcumin to help fight inflammation and an enteric coating to prevent fishy, after-taste burps). Once oils become stagnant, they become the “buffet table” for common skin germs, who feast on the oils, create inflammatory byproducts and lead to the vicious cycle of dry eye disease.
Part 4 focuses more on how to correct this…
Why do some people produce “pasty meibum?” PART 2
Part 2:
Fortunately, not all the tear oils come from the MGs – I quote from (and partially interpret) a scientific publication (below) regarding the composition (and sources) of tear oils.. For those not interested in all of the science, the take home is that much as we regard the Meibomian Glands as the sole provider of tear oil, the reality is that there are other likely sources that make significant contributions. The hopeful news (from my perspective) is that some of these alternative oil sources may be able to be amplified in some cases of reduced (or absent) MG function – to offset the deficiency of the MG dysfunction. I believe I’ve witnessed this in some cases where there do not appear to be any residual MGs left in any of the lids – yet the function of the tears, and general health of the corneas, appear clinically adequate (and may have little-to-no dry eye symptoms) …
"There is no doubt that the meibomian glands are a prominent source of lipids for the TF (Tear Film). However, it would have been a mistake to exclude from consideration other likely sources of lipids (oils), such as conjunctiva, cornea, and AT (Aqueous/watery Tear) produced by lacrimal glands. Earlier publications provided some clues about possible differences in lipid (oil) compositions of MGs and AT and similarities in the AT samples collected using the microcapillaries and Schirmer test strips.27 34 35 Our current HPLC-MS (fancy scientific analyzer) data showed that lipids of aqueous tears are more complex than meibomian gland secretions, necessitating a more cautious interpretation of the roles of the latter in tear film physiology. The observed presence of lower molecular weight compounds with m/zvalues between 500 and 600 and the detection of the large quantities of the compounds with higher polarities than typical meibum components suggest a more complex TFLL (Tear Film Lipid Layer) composition than the one based only on MGs. Therefore, a detailed comparative lipidomic analysis of specimens obtained from different sources, determination of the structures of the newly detected lipid species, and evaluation of their possible physiological roles are in order." (http://www.iovs.org/content/49/9/3779.full) I remain surprised that there has not been further significant research and advancement of knowledge regarding these “alternative producers” of tear oils and look forward to results of such research.
Why do some people produce “pasty meibum?”
Why do some people produce “pasty meibum?” (A Root Cause of MGD that looks like strings of toothpaste or spaghetti - rather than thin, clear oil when expressed from these oil glands. This “clogs” the glands and creates obstruction.)
Some years ago, I was asked by a colleague about why some people produce “pasty meibum.” I wrote a long diatribe and when I saw a related question recently, I dug this answer up and thought I’d share.
Part 1:
Some of my answers would be somewhat modified today. (As most of you know, I’ve published on off label use of RF (radiofrequency) over Lipiflow and for addressing conjunctivochalasis, Zocuwipes over TTO related cleaning and Maxitears over other oils supplements - FD, consulting RF companies, part owner of the eyeThera company that makes the shields I use for RF expression and consultant to the Zocular company making the Zocuwipes).
My 4-part answer attempts to address that million-dollar question.
The Tear Science folks (initially headed by Drs. D. Korb, C. Blackie, et al - but now owned and operated by J&J) would include poor (partial) blinking in that answer, as that appears to be a major cause of stagnation of the oil producing eyelid glands (MGs). When stagnant oil becomes exposed to air, salts and the acidic breakdown products of bacteria and their oil-digesting lipases - it turns to soap and solidifies. Where normal MG (Meibomian Gland) oils are liquid at body temperatures, these harder oily complexes become wax-like and block the glands. The back-pressure appears to induce withering (or else they go on to produce styes). Of some interest is Dr. Korb’s finding that the temperature of the eyelids in patients with Meibomian (oil) Gland Dysfunction (MGD) is "colder" than those who don't have MGD. As far as I know, no one has been able to explain this phenomenon (though Dr. Korb points out that athletes have higher lid temperatures and appear less prone to this disease), but lower temperatures would also lead to solidification and blockage. Dr. Korb demonstrated to me the capillary attraction produced by the lids as they separate after a full blink. This engages the oil squeezed out by the action of the lids coming together with enough pressure to dispense micro-droplets onto the lid margin. Tiny vertical indentations in the lid margin assist in this backward and upward movement of oil - unless a waxy varnish obliterates these little "riverbeds" and occludes the openings. This is one reason I like to “debride” (scrape off) this waxy varnish as a part of my dry eye exam as it aids my diagnosis and may help in treatment of some with serviceable glands that are otherwise “dysfunctioning.”
Part 2 addresses other sources for tear oils and digs into what these oils are.
Doctor, I have a bright red spot on my eye! What do I do now (about a subconjunctival hemorrhage)?
PART 2
Once a blood vessel breaks, the short-term “fix” to limit blood flowing out and “bruising” the white of the eye, is anything that constricts the vessel (so it is letting less blood out).
- Cold is a good constrictor – so a cold compress over the lids.
- Ironically, drops like Lumify (but see above on this).
- Lubrication of the surface, so preservative free artificial tears.
- Light pressure (assuming you can press on the point where the blood is leaking from).
- Avoiding blood thinners (if the bruise feels uncomfortable, taking aspirin, Advil, Aleve or any other blood thinning products – too numerous to list here – will cause blood not to clot and allow for a larger bruise).
- Controlling blood pressure (so poorly controlled blood pressure will force more blood out of the broken vessel). Worry over the bruise might stir up the blood pressure, so try to relax.
My usual advice to a patient with a bright red spot on the white of their eye is –
- Unless there is undue pain, decreased vision or recent surgery on their eye - to relax (& generally – they don’t need to rush in for an eye exam or treatment)
- Stop blood thinners like oral oil supplements for a few days, aspirin (or other blood thinners – UNLESS prescribed by their primary care or heart doctor – then check with them first). Holding strong spices, exercise, and alcohol for a few days as this also helps reduce blood vessel dilation and reduces blood flowing out of the blood vessel.
- If the “bruise” is particularly unsightly, consider wearing an eye shield (or sleep goggles) at night so you are less likely to rub it or press it directly against a pillow in a way that might re-injure the broken vessel. Don’t rub your eye!
- Keep preservative-free artificial tears in the refrigerator and use them every few minutes as soon as you recognize the broken vessel. Once it is clearly not “growing,” then reduce the applications to hourly or less. The direct “cold” will constrict the vessel and sooth the irritation. The lubrication will reduce the friction. If you have a “eye whitening eyedrop” (Like Lumify) on hand, this could be one of the few times it is worth using it in a medical way – but sparingly and only for a day or two, to help stabilize the blood vessel and the clot that stops it from oozing.
- If you recognize it the moment it happens (which is sometimes possible), then closing the lids and gently pressing over that part of the lid covering the area of bruising may help. Unfortunately, if you look around while doing this, then you may be rubbing over the vessel in a way that pumps more blood out – so keeping your eye closed and not moving your eye - while gently pressing for 30 seconds on and 10 seconds off - for a few minutes may help. Using a covered piece of ice to apply the pressure can be somewhat more helpful. After the first 24 hours, ice and cold is generally only useful for comfort and not useful to prevent further bruising.
- If you are doing heavy lifting, coughing, sneezing, straining at bowel movements or vomiting, then the sudden rise in Blood Pressure can “blow out” a blood vessel – and those on the white of your eye are the more “visible.” Controlling BP has already been discussed and holding back on heavy lifting while healing the broken vessel can help. If the coughing is related to a cold or allergies and/or the sneezing is allergic, then something to reduce allergies and coughing can help. Stool softeners, laxatives and a healthy diet can help with straining. Vomiting, if ongoing, may be worth reaching out to your primary care doctor for an “anti-emetic” (a medicine to reduce vomiting).
- If your eye doctor has recommended hot compresses, it is usually best to hold off for 5 days (allowing enough time for healing the vessel before dilating from the heat).
- If your doctor has prescribed a steroid drop for your inflammation, then continuing that drop while nursing the broken blood vessel is worthwhile, as stopping the steroid risks rebound redness. The dilation of the vessels associated with rebound inflammation will cause the broken vessel to also dilate – and possibly to blow out the small clot that stopped the bleeding and allow more bleeding (and bruising) under that clear membrane we call the conjunctiva.
- Most important – report these events to your dry eye specialist so they know this is going on. They usually will recommend treatments designed to improve your ability to produce more – and better – tears to aid in natural lubrication and in the support of the living surface of your eyes. If the conjunctiva has too much laxity and it is apparent that these loose folds are contributing to the breaking of these vessels (& can commonly contribute to dry eye symptoms – see my earlier posts on this) – then they may recommend a surgical repair (I’ve posted on simple plications). Working with a good dry eye specialist is important to all eye health!
Doctor, I have a bright red spot on my eye! What caused it, is it dangerous and what do I do now (about a subconjunctival hemorrhage)?
Broken blood vessels are a commonplace problem all over our bodies - resulting in what we commonly call a bruise. Generally they are not dangerous (though like most things - they can range in cause and in degree.) In rare cases they can be dangerous - so always report them to your eye care provider and call at once if there is significant pain, if they appear in the context of an eye injury or recent eye surgery or are associated with any loss of vision.
Understanding why a blood vessel breaks in the thin, clear, membrane we call the conjunctiva, (what we call a subconjunctival hemorrhage), means also understanding the membrane and the blood vessels in it. There are also several main functions of this membrane that speak to the dry eye issue that don’t directly relate to broken blood vessels but are also key to how we approach overly dilated and breaking blood vessels.
This “saran wrap-like” membrane we call the conjunctiva is supposed to be smooth, moist, clear and “shrink-wrapped” over the underlying white part of the eye (sclera) and over the inner sides of the eyelids. This provides for a smooth, even, and effortless squeegee of the lids, as they go back and forth over the clear “window” (cornea) we see through. It contains cells and tiny glands that make the proteins and some of the moisture that forms the tears that wash over the cornea. It also acts as the “lymph node” of the eye, containing the important defense cells that protect our eyes from pollution, infection and cancers that could come from sun exposure. It is the job of the blood vessels to supply the red blood support for this membrane, so it can do all these jobs.
Irritation – from pollution, infection, injury, allergies, friction – and sadly, yes - DRYNESS – all conspire to create inflammation – our body’s reaction to irritation. This leads to dilation of the blood vessels so that they can deliver more support to the membrane (conjunctiva) – so it can better do its many jobs. This makes the eye look “red” (from the bigger blood vessels carrying the red blood). This pattern is typically red-pencil web-like, as opposed to the broader strokes of red from broken blood vessels. The larger the blood vessel when it breaks, the larger the broad strokes of red from these “hemorrhages” – creating visible bruising.
Without getting too deep into all the sources of inflammation, I can only touch on the many risk factors for breaking blood vessels in the conjunctiva and I’ll stay focused on the common dry eye-related issues. Friction is a common one, as lack of tears – and most frequently, lack of tear oils, leads to more “drag” over the membrane as it tries to “hug” the support underneath. This support over the white of the eye is a fibrous “glue” that functions a bit like living Velcro (Tenon’s tissue). Friction breaks down the fibers and their glue – so the membrane comes loose (conjunctivochalasis – spelled many ways - please see my earlier posts on this). These pleats and folds twist and turn with blinking or from finger rubbing – and the “shearing forces” tear at the blood vessels. The dryness leading up to this can lead to increasing dilation of the blood vessels – so when they tear open, they can spill more blood than thin ones. Anything that causes irritation will lead to inflammation and to growing larger, redder blood vessels (so they can better do their job of supporting the effort of healing, defending, and otherwise taking care of the health of our eyes).
When you apply “vasoconstrictors” (like Lumify, Visine for red eyes, or other eye whitening over the counter products), these drops cause the muscles in the blood vessels to “squeeze” and choke down the blood flow. Less blood means less redness – the point of the eye “whitener.” The longer-term problem with this is several fold:
- these drops themselves contain preservatives – the harsh, toxic chemicals designed to prevent green fuzzy stuff from growing inside the bottle you apply it with. This “hurts” the eye and triggers more inflammation.
- the “squeezing” of the muscles leads to muscle fatigue. When the muscles “relax” the vessels become bigger, because with relaxation of the squeezing muscles, the blood vessel dilates (and carries more blood) – so looks redder – causing a desire to use more of the drops.
- with sustained use, there is a more rapid “wearing off” (tachyphylaxis), so the ability of the drop to do its job becomes less. This leads to a cycle of drop applications where the only winner is the company selling you those drops.
To fight inflammation, we use “anti-inflammatories” – medicines designed to calm the defenses down and allow the blood vessels to return to a more normal state (I have more comprehensive, earlier posts on this). In a healthy eye, these vessels are so small as to be nearly invisible to the casual observer (hence the “white” eyes). The more irritated the eyes are, the redder they become and the stronger the “anti-inflammatory” medication needs to be to counteract the redness (and quite the eye down). Strongest anti-inflammatories are the steroids like difluprednate, prednisone and dexamethasone. Weakest are the Cyclosporine (Restasis, Cequa and the like) and Lifitegrast (Xiidra) groups as well as the non-steroidals similar to aspirin (Advil, Aleve and the like).
The problem with all of these is that unless you are also dealing with the source of inflammation (whatever irritation is triggering it), then this is a Band-Aid approach. As soon as you back off on the anti-inflammatory medication, then the redness tends to bounce right back. Cauterizing blood vessels is a stronger way to curb them – but again, unless you deal with what brought them along to be big, red, angry-looking vessels, then they tend to grow back with a vengeance (because now you’ve really irritated that surface by damaging it, and the blood vessels are what help it to heal).
Long-term use of steroids can thin membranes and blood vessels, making them more fragile. Anything that thins blood (including all aspirin-like products as well as a bevy of other prescriptive and over the counter supplements, medication and even foods and oils) will mean larger bruises and red spots, too.
Finding the undercurrent of irritation and dealing with it directly will usually lead to the best “cure” for redness. Sometimes this is an autoimmune problem. Sometimes it is an allergy or some chronic toxic exposure (like the preservatives in the whiteners – and sadly also the steroids. Fortunately, the cyclosporine and lifitegrast products do not). Sometimes it is from incomplete restoration of the tears and ongoing dryness. The total number of causes of inflammation is a very long list, best sorted out by your dry eye specialist and any team required to turn over every stone and leaf. This means that until every aspect of irritation leading to redness is addressed, then it is hard to effectively reduce that redness. As long as there is friction, irritation and inflammation, this is an uphill battle.
My next post will cover the “what to do’s” when these bruises happen on the white of your eye.
Problems with use and proper care of a Bruder (or similar) moist heat eyelid mask.
As a dry eye specialist who recommends the Bruder masks to my dry eye patients, I like their simplicity, low cost and ease of use. I’ve posted on use of hot, moist compresses before, so this post is more about the Bruder-style mask. I’ve had a few returns for a mask that opens up and bleeds beads in the microwave. There are a few reliable causes, though some do seem to occur spontaneously (most seem to last at least a year or longer with regular use and adequate care).
A few caveats:
- If you wear makeup (especially mascara and/or lid liner), some products contain metals (to give more visual “pop”). Any metal on the mask that goes in the microwave will cause arcing and burn the mask (leaving little or bigger “burn holes” the beads can escape through). Always remove makeup thoroughly before using the mask - or at least use a tissue (or the more expensive disposable covers sold by Bruder and others) to cover the mask when you use it.
- you can gently clean the mask with soapy water and rinse well. Let it fully dry (about a day) before microwaving it again.
- when you have it on for a few minutes and your lids are sufficiently hot, try doing “eyelid crunches” (my term for intermittently squeezing the lids moderately strongly together and then releasing the tension. I find a slow count of “3” on and off squeezing is sufficient if done for a minute or two while the lids are sufficiently warm). This promotes moving the oils that were once cold, thick and “hard” through and out of the glands while the oil is thin and more able to move through the glands.
- avoid heavy pressure over the mask. Light contact with the lids is favored but higher pressure also can put pressure on the eyeballs under the lids (which can raise your eye pressure - not good if you are prone to glaucoma).
- you are likely to notice a feeling of greasy oil in your eyes (that can also be somewhat blurring) for several minutes after you remove the mask (especially if you’ve expelled a good dose of waxy oils).
As usual, consult your dry eye specialist for proper care of your particular condition.
How do everyday products affect our eyes?
When I see patients with complex problems like dry eye disease, allergies or eyelid skin problems (which are often all interrelated), one of the questions that I ask is - what products do you use in or around your eyes? For everyone, this can include contact lenses and the solutions used to clean, disinfect and moisturize them (see my earlier post on that). Various prescriptive and over the counter eye drops gels and ointments are another group. For most, this can also include skin cleansers, moisturizers or sun-blocking creams. This time of year (being the day before Halloween) it might include face paint or theater glues to apply false moustaches and beards. Colored costume contact lenses. For women, this frequently includes various forms of daily makeup, lid liners, mascara and eyelash extensions - yet all of these products may contribute to the eye problems they present with.
There are many posts (mine and others) denouncing “bad products” and I point out to my patients that in the USA, there is little governance overseeing producers of makeup (EWG offers free online information and is one of a few online consumer protection groups that target makeup and other everyday products that can be bad for you. I quote from some of their online information found here: https://www.ewg.org/news-insights/news/2021/08/protecting-consumers-toxics-cosmetics-us-lags-least-80-countries ). In some countries there are over 1600 ingredients banned from makeup as opposed to just 9 banned by the FDA from makeup for safety concerns and 80 countries lead us (in the USA) in banning harmful chemicals in makeup products.
Once this information is absorbed by our brains, we might pooh pooh it by thinking “my products are:” “all natural” or “organic” or “vegan” or on the label it says “doctor tested and doctor approved.” But what does this really mean? In the USA, it usually doesn’t mean much, since there is so. little oversight to hold these companies accountable - and just because the company has a “big name” or “great reputation” (as in “even my grandmother used this stuff” and “all my friends say it’s great”) - unfortunately these statements can all be false or misleading.
A young patient of mine was recently referred because she had severe scarring of her corneas that was an imminent threat to her vision. She was studying about cosmetics and wore eyelash extensions - which looked great - but her mother stated that her eyes were “blood red” for several hours each time she had them applied. She wore contact lenses that were cleaned daily in an “all purpose” solution and she had makeup on that raised more concerns. Basically, each of these alone might cause a problem like hers, but together, were likely the “perfect storm” to cause this eyesight-threatening scarring. Add to that the usual dry eye problems common to all school-aged children and young adults (again see my earlier posts) - and she was in grave dangers that may haunt her the rest of her (likely long) life.
Why is it so hard to protect people from unscrupulous companies that use toxins in their products and then prey on the public when they hard-sell those products to us? The answer goes beyond the weakness of our political leaders (though this is an obvious start to the fix). As long as corporate dollars can sway the politicians elected by us to protect us, I think we can be sure that our best interests are not sufficiently protected. But that is not the whole answer. Unfortunately once you start adding chemicals and their compounds to other chemicals, the resulting mix can become much better - or much worse - as sum of their parts - than any one or two taken alone or together. This concept was put most articulately in digital ink by my friend, brilliant colleague and lid hygiene product inventor, Peter Pham, MD. Dr. Pham is the inventor or the Zocular lid care products I’ve recommended for years to my patients. He majored in chemistry before going on to his MD degree and then to a career in ophthalmology where he practices in Texas. His recent post to a group of dry eye doctors is quoted here:
“The ingredient list is a whole lot more than the sum of its parts. It's too confusing to try to deduce "goodness" or "badness" from any individual ingredient. A better approach is to understand the purpose of an ingredient or set of ingredients. Is it there to emulsify? Chelate metal ions? Balance pH? Provide bulk? If an ingredient serves a purpose, it's less likely to cause harm - if we grasp the steering wheel with both hands, it's hard to punch our passengers. Similarly, if a hydroxyl group forms hydrogen bonding to another compound, it can't chase a different compound. Chemicals, like hands, can be used to harm or help. Attempts to avoid certain chemicals often abolishes entire classes of molecules that can actually help our patients, and alternatives that appear more organic or pure can have unexpected, unknown properties since there's little data or experience with newer compounds. As an example, EWG classifies behenyl behenate as a safe "1" even though there's no data to support or refute this. As another example, many blogs suggest "alcohols" should be avoided in a formulation with little discussion about the nuances of "alcohol". This would basically remove classes of alcohols that moisturize, preserve, emulsify, etc. And includes one that intoxicates, which feeds into our fear of "alcohol". If it fries our brain with just a few sips, what would it do to our eyes!
To add to the complexity of trying to divine poison or cure from an ingredient list, the list itself is only a partial list of ingredients since many of the listed ingredients have its own set of ingredients that aren't listed. As an example, most surfactants come as a liquid concentrate. This concentrate has its own list of ingredients - stabilizers, preservatives, etc. Listing the ingredients within ingredients of ingredients would make a novel and add little to our ability to predict or understand a formulation.
There is no risk-free activity in life. The very oxygen that gives us life will lead to our demise through secondary oxidative processes. But we should avoid obvious dangers like putting microscopic arrows in a formulation like Laura M Periman said.”
So should we just give up and let the free market determine what products we use? My answer is a hard “NO” and is based on almost 40 years of clinical practice and training. I advocate that we educate ourselves on what is generally known (using apps like “EWG” and “Think Dirty, Shop Clean” - however imperfect they may be), that we listen to the advice of those more medically knowledgeable, like our dry eye specialists and dermatologists and we invest public dollars into research so we can better learn the nuances of how safe or how risky these daily products can be. Meanwhile, use caution and remember that beauty is in the eyes of the beholder. We all have an inner beauty that can be revealed through our actions - and does not necessarily require products to hide what we perceive to be imperfections. Stay safe.
What’s new in treating Blepharitis?
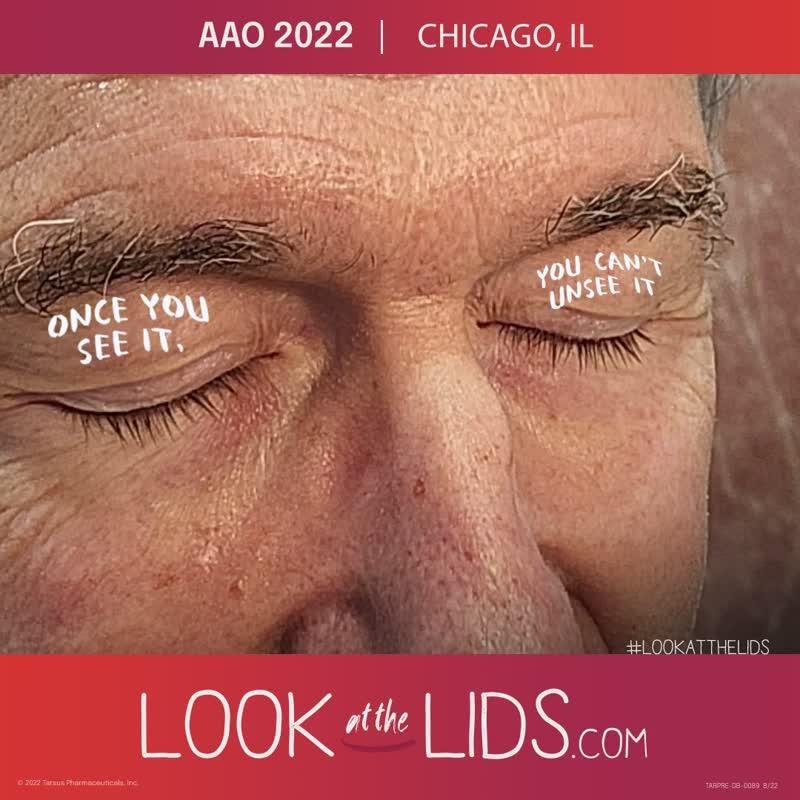
During my time at the national eye meeting in Chicago earlier this month, there was a big focus on a new treatment for Demodex-related blepharitis. At the booth representing Tarsus - the company making this new treatment medication, they offered to take pictures of attendees - so I naturally volunteered. Yes, the awful photo of my face titled “AAO 2022 / Chicago, IL” is what you see below. Fortunately, my eyelids looked quite clean (thanks to my daily routine of Zocuwipes and Avenova lid hygiene - I’ve posted on this earlier) - though my face shows off my significant rosacea, fine lines and extra skin - called dermatochalasis - which basically means I’m overdue for my IPL and RadioFrequency lid treatments.
The photo beneath my photo is of a patient’s eyelids that I took through the eyepiece of my office slitlamp (a kind of microscope we eye doctors use to help us examine our eye patients). That poor patient has a lot of blepharitis - and the waxy “collars” around the base of the lashes illustrates the typical finding we see in eyelids that are “colonized” (in this case, overrun) with Demodex - the tiny skin mite that commonly lives in and around eyelashes. They subsist off eyelid oils and germs that live off our tears. Unfortunately, they are quite prevalent (if you go by age, the likelihood that you will carry these mites goes up approximately 10% per decade - so by age 50, you have a 50:50 chance you have them - and by that equation, by age 100, you would be certain to have them) - but as with all statistics - it only matters if it affects you.
If you have these mites - and if you have resistant skin, then you may not know you have them - you might not care - and it might not matter. However, if you have sensitive skin (common in ocular rosacea, like I have), then the life cycle (which I won’t get into, as it would likely keep you up all night like a bad horror movie) is likely to be like adding gasoline to a flame. This causes irritation that leads to inflammation that fans the flames of dry eye disease. Tarsus is repurposing a veterinarian medicine (used to treat dog’s mange) as this medicine has proven extremely effective at knocking off this mite without irritating human eyes or eyelids. Sadly, it is likely to take months (and could be closer to a year) before it passes through the hoops of the FDA and becomes something we eye doctors can prescribe for our patients.
The good news is that there are many treatment options that are already available and can be quite effective. In fact, the BlephEx and ZEST treatments many dry eye specialists use, coupled with ongoing Zocuwipe (or some Tea Tree Oil or TTO-derivative products like Cliradex) and Hypochlorous Acid sprays (like the pure version in Avenova) that I personally prefer (and use) are generally capable of controlling if not eradicating these mites. IPL has also shown good efficacy (see more of my posts on this) and off label use of Ivermectin cream are extra tools we already have. Still, I look forward to another powerful tool to help more of my patients - as insurance companies are yet to cover lid hygiene treatments like BlephEx and ZEST, don’t generally cover IPL, and don’t like us to prescribe off label treatments - so once this new drop is approved by the FDA for this specific indication, it is that much more likely to be covered by insurance - making it more available and affordable for most!
My IPL Demo and “Pearls” for optimal treatment.
The following IPL video (at the bottom of this post) shows me performing a most basic IPL treatment for dry eye disease. Many patients might be better served with a fuller face treatment than shown here, but for a quick maintenance treatment - especially in the time of a pandemic, this can suffice. What makes an IPL treatment most effective depends on what the goals for that IPL treatment might be and each patient’s care should be customized to best achieve those goals.
One of the most common reasons for dry eyes today, is obstructive Meibomian Gland Dysfunction - or “o-MGD” - the clogging of the oil-producing glands of the eyelids. Oil is a key ingredient of a healthy tear - as I’ve blogged before. If this is the primary problem being addressed with IPL, I find IPL relatively inefficient and often ineffective, as the brief heating achieved by the light is quickly dissipated. This allows the oil to go from solid (cold) to liquid (hot) and then rapidly back to cold (solid) as the skin cools - so the ability to effectively express the oil from these glands becomes harder as the oil itself gets harder (in consistency). For the few patients where clogging is the single significant issue, a simpler heated expression can offer a better alternative.
One of the other common reasons for dry eye is inflammation (from the many causes I’ve covered in past posts). Inflammation is the body’s reaction to irritation and comes via dilated blood vessels - delivering “hot blooded fighters” - our body’s defense - including what I refer to as our “Napalm, bullets and handgrenades” - ammo that we use to fight the most significant, long-term enemies of human life —- germs. The problem with this warfare is that all this ammo spews onto the surface of our eyes and inadvertently “beats up” on the tiny tear glands trying to make healthy tears. IPL is a great solution to this problem. The light can reduce and even close the red, angry blood vessels, so less ammo is delivered. The light also can kill off many of the germs that often contribute to the calling of the defenses - while also stimulating the cells of the glands that make the tears. Yes - it can also heat the oils - so when the oils are not particularly solid - so the glands are not especially clogged - it can help with some of the oil’s flow. When the blood vessels dilate, they can creep up from deeper levels and “bloom” into the lids and then into the tears. IPL can “prune back” this “tree of inflammation.”
When the blood vessels flare, this qualifies as what we dry eye doctors call ocular rosacea. IPL is like a “silver bullet” if used properly to treat this.
So what are the key things one needs to know to get the best out of IPL for this indication?
Remember that the darker the color of skin, the more “pigment” (or color) will get in the way of treating the blood vessels that largely lie below. The primary driver of color comes from your genes and exposure to sun (or any UV) light. Being careful to sun “block” (proper clothing, sunscreen) will help reduce production and if skin is darker than ideal, consideration can be made for skin lighteners (Kojic Acid, Hydroquinone and others) - so that the IPL can do its best against the inflammation-bearing vessels.
The biology of how IPL works on causing blood vessels to “retreat” is to slightly (on purpose) damage them and then allow the body to heal (reabsorbing the damaged ends of the vessels - which causes them to effectively “retreat”). The time course for this regression starts on the day of the IPL (the red blood color is the “target” of the light and causes the vessels to contract, the blood to clot the roughened inner lining to “stick” together with this clotted “glue.” Typically, the damage begins to heal over the first 3 to 5 days and continues over another 3 to 4 weeks. To best take advantage of this healing process, it helps to follow a few basic steps -
Prior to your treatment, avoiding tanning (including tanning lotions) helps the IPL do its best work (as noted above). Avoiding blood thinners that are not required for your medical health may help (consult with your doctor(s) before stopping any blood thinners). Controlling blood pressure can help, too.
Immediately following your treatment, cool compresses (off and on until the skin effectively cools down) can help in shrinking the damaged vessels and help sooth the intentionally injured skin. Extra care to avoid sunburning/sun tanning is important as IPL - while not containing UV - is still light - and your skin is now damaged. Adding UV from any source (like sun or tanning beds) can add to that damage (and also promote tanning).
For the following 3-5 days, avoidance of anything that will dilate blood vessels (causing skin “flushing”) will also work towards closing those blood vessels (flushing pushes blood through the damaged, blood-clotted vessels and keeps blood flowing in ways that can promote the regrowth and extension of these unwanted vessels). This includes excess physical activity (exercising), hot showers, saunas, alcohol and spicy foods among others. If you’ve noticed anything you do that causes flushing, I’d advise against it during this key time where blood is clotting and closing off these vessels from light-related injury.
The ideal “window” for the next treatment appears to be in the range of 3-5 weeks. for most patients attempting to reduce their ocular rosacea. Less than 2 weeks means the “bad” blood vessels have yet to fully heal and “regress” - so treating too early can mean there isn’t enough time to get the full benefit of the earlier treatment session. Waiting beyond 6 weeks appears to give the “bad” blood vessels enough time to regenerate - or grow back - so this is a bit like a dog chasing its tail (and not getting anywhere from all that effort). Catching the vessels at the ideal moment when the healing has fully occurred - but before they begin to come back - is the ideal, but sometimes difficult goal. Age, medications, medical problems and genetics all play a role in how quickly we heal - so sometimes your IPL provider may have to use apparent progress as a means to determine the best spacing of treatments.
The number of treatments required will vary depending on the size and distribution of the “bad” blood vessels, the energy and dynamics of how the light is applied, the degree to which these prescribed recommendations are followed, the extent of the problems caused by the ocular rosacea to the glands and tissues of the lids and eyes, genetics, environment, age and probably countless other issues. The average number of consecutive treatment sessions in my practice averages around 4 before we re-evaluate and for most, there will be “maintenance” treatment sessions of 1 or 2 per year (also depending on all the above).
Ancillary treatments (LID HYGIENE, heated expressions, and the “usual homework” I prescribe can greatly affect the effectiveness of IPL treatments. Other co-contributors to dry eye disease can include deeper levels of obstruction (including harder degrees of clogging from keratin and scar tissue) may require Maskin Probing while co-contributors like allergies, lid problems like inturning, out-turning, poor closing and general laxity - and my favorite - conjunctival chalasis - have generally been covered in my earlier posts (though I expect to continue refining and updating these posts to help keep them current and relevant).
MY IPL DEMO IS LINKED HERE:
https://heycool.wistia.com/medias/pwj9sns0wj
What makes “enough,” ENOUGH and is there such a thing as “too much?” PART 3
First, I want to apologize for not posting last weekend - I was in Chicago at the annual national eye convention (put on by the American Academy of Ophthalmology) that is actually a global convention and is generally considered to be at the top of the world’s educational system for eye surgeons. I have never come away from one of these meetings without learning something - as the newest medications, technologies and best “look into the future” is commonly saved to present during these events. I’ve had to miss the last few of these meetings in person due to the pandemic, but I did tune in virtually and was happy to learn from some of the best. I will reveal some of what I learned in future blog posts - but today, I want to pick up where I left off on what makes “enough,” ENOUGH!
So is there such a thing as too much antibiotics (like Doxycycline or Azithromycin) for fighting dry eye-related infections and inflammations? The short answer is yes - as these can change out bad germs (resistant) for good germs (that promote good health) as antibiotics don’t know the difference between good germs and bad - they just wipe out whatever germs are susceptible. They also can cause other side effects (too numerous to cover in full - and each patient’s case should be carefully considered by the treating doctor so as to avoid predictable bad outcomes) and can sometimes provoke allergies to antibiotics across the class (so small doses even for short times may leave certain patients unable to ever take any similar-class antibiotics for life). This is not to say that all antibiotics are “bad” - just that all antibiotics should be carefully considered in the context of each patient before prescribing them. In general, good lid hygiene can go a long way towards avoiding eye and eyelid infections (see my earlier posts).
How about treatments like IPL and heated expressions?
Taking IPL first, while this is a terrific treatment for most with dry eye disease, there are limits to what it can treat and the strong suit is inflammation. Unless the root of inflammation is understood (and is in the wheelhouse of what IPL can treat), then while IPL may have some short-term benefits, it is possible that it will wear off sooner than later and by delaying progression, it may cloud the ability to determine the driver of this inflammation (and delay the ultimate treatment). It also can have diminishing returns at some point, so success should be periodically measured and future treatments should be planned according to the rate and degree of that success. Poor, but steady progress may mean staying on course until a plateau is reached. Small steps forward, followed by equal steps backward may mean it is time to completely re-evaluate the treatment strategies. Maintenance is almost always required and timing those extra treatments can also be critical to avoiding larger steps backwards and lead to greater needs for multiple sessions to gain back that lost ground. Too much IPL is when it is no longer helping or when it is being used as a crutch without fixing the main drivers of the disease.
Heated expression is likewise a terrific treatment - but only when it is up to the task of melting the obstructions and then adequately expressing them. If the waxy clogging is of a melting point higher than the heat used - then a liquid form of the oil is never achieved and the ability to express is negated. Once liquid, if the amount of pressure used to express is not sufficient to adequately purge these liquid oils from the glands, then once the heat stops, the oil cools and turns solid again - blocking the glands and leaving insufficient treatment benefits. If the clogging is from dense, non-waxy products like keratin or scar tissue, then heat and expression pressure alone is not the answer. These cases may better respond to Maskin Probing - often in concert with some or all of these light and heat technologies (see my earlier posting on this). Once the waxy products are fully expressed, then heated expression may still have some value (purging the subsequent oil gland products that may still be less healthy and making room for newer, fresher, healthier oils to be made and expressed with normal, strong blinking. At some point, this will also plateau in benefits and will commonly have diminishing benefits as that plateau approaches. Too much heated expression (be it Lipiflow, iLuc, TearCare, Mibo or my favorite off label use of radiofrequency) is when it isn’t working.
As I usually say, each case needs to be evaluated carefully and treatments picked logically.More important is the ongoing evaluation of treatment progress and then re-evaluating - as the twists and turns of the road are uncovered. Picking dry eye specialists who have a full range of diagnostic equipment and treatment options is also almost as important as finding one with a good education and experience. Heeding their advice and working closely together is likely to yield the greatest results. Find a good dry eye doctor.
What makes “enough,” ENOUGH and is there such a thing as “too much?” PART 2
What about Lid Hygiene - what’s “enough?”
I think of the lid a bit like a dentist looks at teeth. Scraping the lid margins (I usually use the cut end of a wooden cotton tip applicator, but various metal “scrapers” exist for this purpose) is a bit like removing tartar from teeth. Mechanical (like BlephEx) or vigorous scrubbing (like ZEST - I like a hybrid of BlephEx and ZEST) can remove the remaining “plaque” (what eye doctors call scurf). Some keratin (the tough stuff that also makes up fingernails and hair) along with waxy debris is commonly removed with the “scraping” and it is often possible to express oils a little better after just these lid hygiene maneuvers. Heated expression is generally needed to unclog deeper plugs and probing if there’s much scarring.
There appears to be at least 3 forms of obstruction: keratin, scarring and wax (& probably various combinations of all 3). As glands clog, they also wither (atrophy). Ideally, we will have answers for all of this, but the best is getting early care and addressing issues earlier. I find combination therapy (debridement or “scrapping” for superficial keratin and wax, heated expression for deeper wax, Maskin probing for scars, keratin and waxy residue. Currently we have IPL, “homework” and anti-inflammatories for rejuvenation (anti-withering). Homework is usually pretty straightforward in terms of adequate hydration, Omegas, strong, regular blinking, lid hygiene, and most often, warm moist compresses - but can include other treatments depending on clinical course and findings (& maintenance treatments as needed). How and where a new selenium-based (AZR 001) ointment will fit in the protocols we have is, in my limited knowledge of the information available, still yet to be determined. I’m all for adding arrows to my quiver of treatments, so will stay tuned to this one. See my posts on lid hygiene for a deeper dive.
For “super sensitive skin” there are times when even weak Hypochlorous Acid (Like Avenova) can irritate and Tea Tree Oil-based products are usually even more irritating. The Okra-based Zocugel and Zocuwipe cleaners tend to be less irritating but each patient is different and sometimes less is more. Finding the balance that keeps lids clean (and reduces the inflammation from germs that otherwise can signal inflammation to increase) is a job best left between you and your dry eye specialist. Oral medications (like Doxycycline or Azithromycin - available topically as well as orally) and treatments like IPL can also help to reduce the germ burden and reduce inflammation without directly irritating skin (see my posts on these options).